The biopsychosocial model (BPSM) is a comprehensive framework that explains how biological, psychological, and social factors interact to influence health and illness.
Xiao et al. 2021 in “Analysis of Real-World Implementation of the Biopsychosocial Approach to Healthcare: Evidence From a Combination of Qualitative and Quantitative Methods” found medical staff had only a 37.5% chance of addressing psychosocial status, showing underuse of the model, underscoring the need to strengthen biopsychosocial practices.
The components of the biopsychosocial model encompass biological influences, such as genetics and physical health, psychological elements, including emotions and coping strategies, and social aspects, including family, culture, and socioeconomic conditions.
The application of the model spans chronic illness care, mental health treatment, pain management, addiction recovery, rehabilitation, and preventive healthcare, offering a holistic framework that considers multiple determinants of health.
The strengths lie in its holistic perspective, patient-centred approach, improved treatment adherence, and adaptability across medical and psychological disciplines.
The limitations involve the complexity of assessing diverse factors, the subjectivity of psychological and social variables, and challenges in integrating the model within healthcare systems that prioritise quick biomedical solutions.
What Is the Biopsychosocial Model?
The biopsychosocial model is a theoretical approach introduced by psychiatrist George L. Engel in 1977. Engel challenged the reductionist biomedical model by emphasising that illness is not merely the consequence of biological dysfunction but also shaped by cognitive, emotional, and social dynamics. The theory is used to explain both the onset and progression of health conditions, as well as recovery processes.
In “Biopsychosocial-Based Exercise Model for Rheumatic Diseases”, researchers showed that a 12-week Biopsychosocial-Based Exercise Therapy (BETY) program significantly bolstered outcomes for people with rheumatic conditions. Participants reported better physical function, reduced fatigue, improved mood, stronger social participation, better sleep, and enhanced sexual health compared to control groups, confirming BETY’s effectiveness in ameliorating overall quality of life.
What Are the Key Components of the Biopsychosocial Model?
The key components of the BPSM are biological, psychological, and social factors, each shaping health in distinct ways, and are explained as follows:
Biological Factors
Biological factors represent physical and genetic aspects of health. These are genetics, brain chemistry, immune function, hormones, organ health, and physical injuries. For example, a person with a family history of diabetes is biologically predisposed to developing the condition.
Psychological Factors
Psychological factors encompass mental processes, emotions, and behaviours that influence health. This consists of coping mechanisms, personality traits, stress responses, thought patterns, and mental disorders such as depression or anxiety. For instance, chronic stress worsens cardiovascular disease by elevating blood pressure.
Social Factors
Social factors involve environmental and cultural influences that affect health. These cover family support, socioeconomic status, employment, education, cultural beliefs, and access to healthcare. For example, a person living in poverty faces a higher risk of illness due to limited resources, poor nutrition, and inadequate medical care.
How the Biopsychosocial Model Differs from the Biomedical Model
The biomedical model focuses primarily on diagnosing and treating biological dysfunctions such as pathogens, organ failure, or genetic abnormalities. Although effective for acute conditions, it overlooks the role of psychological resilience and social determinants in recovery.
The biopsychosocial model expands this perspective by integrating mental and social domains. This allows healthcare providers to treat not just the disease but the person as a whole. For example, in treating chronic pain, the biomedical model relies on medications alone, whereas the biopsychosocial model incorporates counselling, stress reduction strategies, and social support to improve outcomes.
Alagappan et al. 2025 in “Knowledge, Attitude and Practice of the Biopsychosocial Model in Chronic Musculoskeletal Pain Management among Physiotherapists” surveyed 116 Indian physiotherapists and discovered strong theoretical knowledge and positive attitudes toward the BPSM, with awareness averaging above 4 on a 5-point scale and broad willingness for further training and interdisciplinary work. Yet, practical use was limited by time pressures, patient non-compliance, and resource constraints, leaving biomedical approaches dominant despite theoretical support for the model.
What Are the Applications of the Biopsychosocial Model?
The applications of BPSM are broad, extending across chronic illness care, mental health treatment, pain management, addiction recovery, rehabilitation, and preventive healthcare, and are discussed below:
1. Chronic Illness Management
Chronic diseases such as diabetes, hypertension, and arthritis require more than medication. Behavioural changes, emotional adaptation, and social support are central to long-term management. Physicians use the biopsychosocial framework to help patients develop healthy routines, manage stress, and build supportive networks.
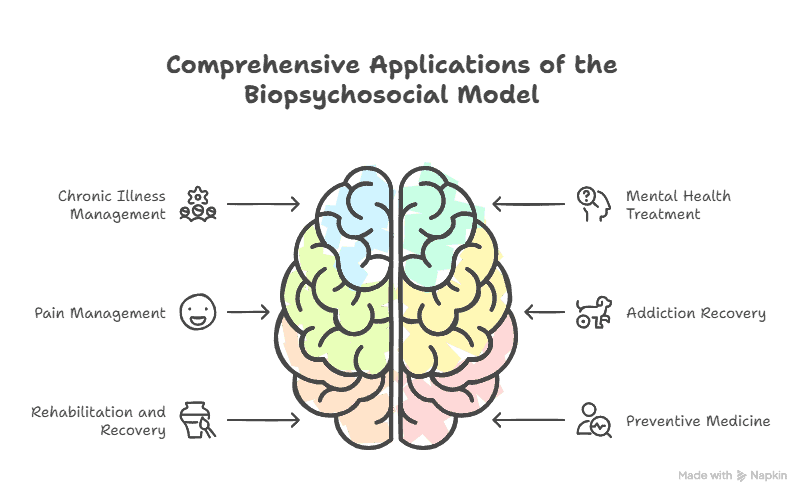
2. Mental Health Treatment
In psychiatry and psychology, the model is essential for understanding disorders like depression, anxiety, and schizophrenia. Biological factors such as neurotransmitter imbalances are addressed alongside cognitive therapy and family or community support systems.
3. Pain Management
Chronic pain is influenced by physical injury, emotional distress, and social context. Pain specialists apply biopsychosocial strategies by combining medication, physical therapy, mindfulness techniques, and social interventions such as workplace adjustments.
4. Addiction and Substance Use Disorders
Addiction treatment demonstrates the strength of this model. Biological predispositions (genetics, brain changes), psychological triggers (stress, trauma), and social influences (peer pressure, family environment) all contribute to substance use. Effective de-addiction rehabilitation integrates detox, therapy, and community support systems.
5. Rehabilitation and Recovery
Patients recovering from strokes, spinal cord injuries, or surgeries benefit from this model because it integrates physical rehabilitation with mental health support and social reintegration, bettering quality of life.
6. Preventive Medicine
Preventive healthcare uses the biopsychosocial approach by encouraging lifestyle changes, stress management, and community-based health promotion programs. Vaccinations and screenings are paired with education and social outreach to increase effectiveness.
What Are the Strengths of the Biopsychosocial Model?
The strengths of the BPSM are its holistic perspective, patient-centred approach, improved treatment adherence, and adaptability across disciplines, and are explained below:
- Holistic perspective: By considering biological, psychological, and social factors together, the model provides a more complete understanding of health and illness.
- Patient-centred approach: Treatment is tailored to the individual, promoting active participation and shared decision-making.
- Better adherence: Addressing emotional and social needs alongside medical care increases patient engagement and long-term compliance with treatment.
- Cross-disciplinary adaptability: The model is effective across medicine, psychology, psychiatry, social work, rehabilitation, and public health, making it versatile in diverse care settings
What Are the Limitations of the Biopsychosocial Model?
The limitations of the BPSM model are complexity in assessment, subjectivity in measuring psychosocial factors, and challenges in healthcare integration, and are elaborated in the following:
- Complexity in assessment: Evaluating biological, psychological, and social variables together requires more time, detailed tools, and multidisciplinary input, making it harder to apply in fast-paced clinical settings.
- Subjectivity in measurement: Psychological and social influences are less precise than biological markers, creating variability in diagnosis and treatment planning.
- Challenges in healthcare integration: Many healthcare systems prioritise quick biomedical interventions, limiting resources and support for adopting a comprehensive biopsychosocial approach.
- Incomplete adoption in practice: Evidence shows that despite theoretical acceptance, practical application is inconsistent, with biomedical approaches still dominating in routine care.
How is the Biopsychosocial Model Applied in Clinical Practice?
The biopsychosocial model is applied in clinical practice in the following ways:
Assessment
Clinicians assess patients by exploring:
- Biological history (genetics, medical conditions, medications)
- Psychological status (thought patterns, stress levels, coping strategies)
- Social context (family, employment, culture, community)
Treatment Planning
Based on assessment, treatment plans integrate medication, psychotherapy, lifestyle interventions, and social services. For example, a patient with hypertension receives antihypertensive drugs, stress management therapy, and nutritional counselling.
Patient Involvement
The model encourages active participation of patients in their recovery process, strengthening self-efficacy and long-term compliance with treatment recommendations.
What Is the Role of the Biopsychosocial Model in Modern Healthcare?
The role of the biopsychosocial model in modern healthcare is to blend biological, psychological, and social factors into patient care, creating a holistic and patient-centred approach.
It supports chronic disease management, mental health treatment, pain rehabilitation, and preventive care through multidisciplinary collaboration. With the rise of digital health and telemedicine, the model also enables real-time tracking of physical, emotional, and social indicators, strengthening customised medicine and boosting outcomes.