De-addiction is the structured practice of overcoming dependence on substances such as alcohol, drugs, or behavioural addictions through medical treatment, psychological therapy, and social support.
The Indian Ministry of Social Justice and Empowerment partners with state governments, NGOs, and voluntary organisations to establish and operate Integrated Rehabilitation Centres for Addicts (IRCAs), Community-based Peer Led Interventions (CPLI), Outreach and Drop-In Centres, and District De-addiction Centres. In addition, around 66 Addiction Treatment Facilities (ATFs) have been set up within government hospitals to expand access to structured treatment and rehabilitation services.
De-addiction is important because untreated addiction brings about severe health complications, social isolation, financial distress, and even premature death.
The process of de-addiction involves multiple stages, including detoxification, counselling, behavioural therapies, medication-assisted treatment, and long-term rehabilitation.
Challenges such as relapse, stigma, non-ethical admissions, and lack of access to specialised facilities make recovery difficult.
Preventive strategies and relapse management are therefore critical for sustained sobriety, making de-addiction not only a personal journey but also a public health priority.
Since addiction affects brain chemistry, relationships, and society at large, de-addiction programs are vital for breaking cycles of dependence and supporting recovery.
What Is De-Addiction?
De-addiction is the therapeutic process of ending substance dependence while treating the psychological, social, and physical consequences of addiction. The measure involves medical detoxification, rehabilitation programs, therapy, counselling, and peer support groups. The primary aim is not only to stop substance use but also to empower individuals to regain control of their lives and prevent relapse.
The National Survey on Extent and Pattern of Substance Use in India (2019) by the Ministry of Social Justice and Empowerment revealed alarming trends. About 160 million people (14.6%) aged 10-75 consume alcohol, with 5.2% dependent on it. Cannabis use affects 31 million individuals, while 0.66% face cannabis-related disorders. Opioid consumption is seen in 20 million people (2.1%), with 5.5 million requiring treatment. A parallel household survey estimated 62.5 million alcohol users, 8.75 million cannabis users, 2 million opiate users, and 0.6 million sedative users, of whom 17-26% were dependent and in urgent need of intervention.
Why Is De-Addiction Important?
De-addiction is important because it:
- Prevents severe health consequences such as liver disease, heart complications, and mental health disorders.
- Lowers the chances of accidents, violence, and crime linked to substance use.
- Restores family stability and strengthens social relationships.
- Improves workplace productivity and reduces the economic burden of healthcare costs and lost income.
- Enables individuals to regain control of their lives, fostering dignity, self-reliance, and long-term recovery.
De-addiction treats addiction as a medical condition rather than a moral failing and ensures compassionate care and sustainable recovery.
What Is the Process of De-Addiction?
The process of de-addiction involves medical detox to safely remove substances and manage withdrawal, followed by rehabilitation programs combining counselling, behavioural therapies like CBT, and, when needed, medication-assisted treatment to reduce cravings. Support systems, including group therapy, family sessions, and 12-step programs, help build accountability, while aftercare planning caters to ongoing relapse prevention and community-based support, making recovery a continuous, systemised journey.
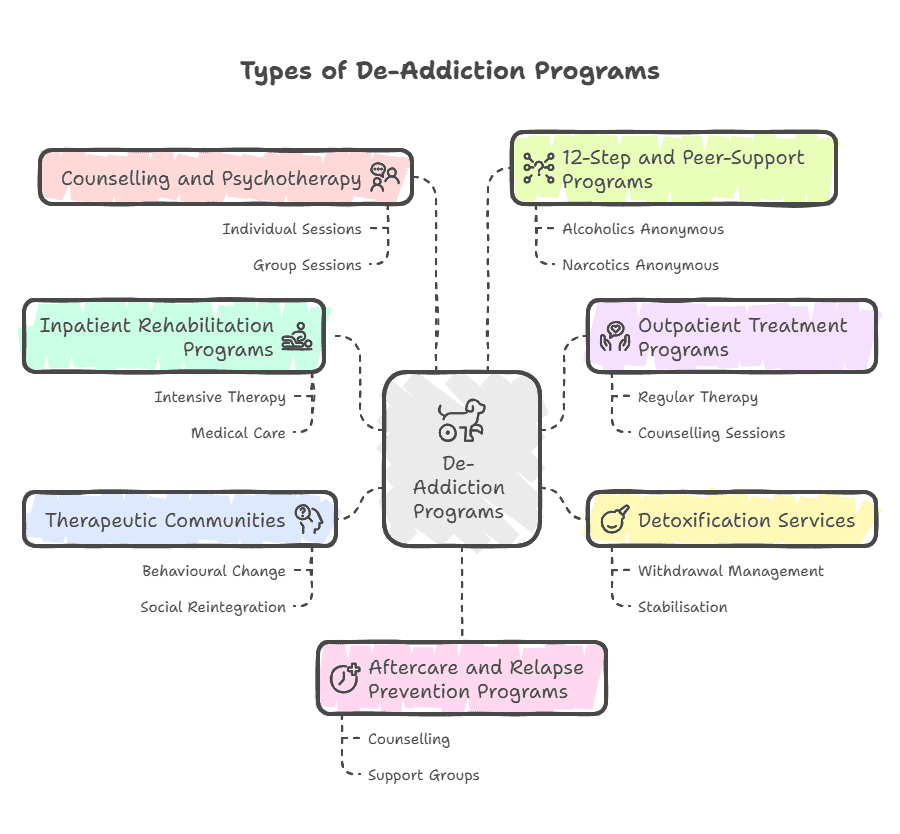
What Are the Types of De-Addiction Programs?
The different types of de-addiction programs are explained below:
Inpatient Rehabilitation Programs
Coordinated, residential programs at rehab centers offering intensive therapy, medical care/
Outpatient Treatment Programs
Flexible programs allowing individuals to live at home while attending regular therapy and counselling sessions.
Detoxification Services
Medically supervised services designed to manage withdrawal symptoms and stabilise individuals before further treatment.
Therapeutic Communities
Long-term, residential setups focusing on behavioural change, peer support, and social reintegration.
Counselling and Psychotherapy
Individual, group, or family-based sessions addressing psychological, emotional, and behavioural aspects of addiction.
12-Step and Peer-Support Programs
Community-based programs like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA) promote mutual support and long-term recovery.
Aftercare and Relapse Prevention Programs
Follow-up care, including counselling, support groups, and skill-building, to prevent relapse.
How Does Medical Detox Work?
Medical detox works by safely managing withdrawal symptoms that occur when an individual stops using addictive substances. The procedure begins with an evaluation to assess the type and severity of substance use, followed by stabilisation through medications, fluids, and medical supervision to reduce discomfort and risks.
During detox, healthcare professionals monitor vital signs, address complications, and provide supportive care. The goal is to prepare the individual physically and mentally for ongoing treatment, as detox alone does not address the psychological aspects of addiction but serves as the critical first step in the recovery process.
What Behavioural Therapies Are Used in De-Addiction?
The main behavioural therapies used in de-addiction are:
- Cognitive Behavioural Therapy (CBT): Empowers individuals to identify and change negative thought patterns and behaviours linked to substance use.
- Motivational Interviewing (MI): Strengthens personal motivation and commitment to recovery by resolving ambivalence about quitting.
- Contingency Management (CM): Uses rewards or incentives to reinforce positive behaviours such as staying drug-free.
- 12-Step Facilitation Therapy: Encourages participation in mutual-support groups like Alcoholics Anonymous or Narcotics Anonymous.
- Family Therapy: Involves family members to bolster communication, resolve conflicts, and strengthen support systems.
- Group Therapy: Delivers peer support, shared experiences, and accountability within a therapeutic setting.
Are Medications Used in De-Addiction?
Yes, medications support de-addiction by reducing withdrawal symptoms, curbing cravings, and preventing relapse. The medicines used in de-addiction are indicated below:
- Alcohol Addiction: Disulfiram (causes unpleasant reaction when alcohol is consumed), Naltrexone (blocks euphoric effects).
- Opioid Addiction: Methadone, Buprenorphine, and Naltrexone stabilize brain chemistry.
- Nicotine Addiction: Nicotine replacement therapies, Varenicline, and Bupropion aid cessation.
- Prescription Drug Addiction: Tapering strategies with medical monitoring, sometimes supported by medications for anxiety or sleep.
The combination of medication and therapy is known as Medication-Assisted Treatment (MAT).
What Are Common Challenges in De-Addiction?
The common challenges in de-addiction encompass relapse attributable to strong cravings, co-occurring mental health disorders, limited access to quality treatment centres, and social stigma that discourages individuals from seeking assistance.
Ethical and professional concerns remain substantial, covering detention without consent in about 31% of centres inspected and physical abuse in about 51% of centres during reported inspections, as detailed by Joseph S. & Hemalatha K. 2021 in “Addiction Treatment in India: Legal, Ethical and Professional Concerns Reported in the Media.”
Bad ethical practices such as unregulated detox programs, overprescription, or lack of professional oversight compromise recovery outcomes and patient safety. The path to recovery is not linear.
Overcoming these requires a strong support system, consistent therapy, and community engagement.
What Role Does Aftercare Play in De-Addiction?
The role that aftercare plays in de-addiction is foundational for sustaining long-term recovery. Aftercare programs offer ongoing counselling, support groups, relapse prevention strategies, and medical monitoring, aiding individuals in navigating triggers and maintaining sobriety. By ensuring a defined follow-up and reinforcing healthy routines, aftercare diminishes the risk of relapse, strengthens coping mechanisms, and ensures that recovery goes beyond the initial treatment phase. Without aftercare, individuals are at high risk of returning to substance use.
How to Choose a Good De-Addiction Centre?
To choose a good de-addiction centre, do the following:
- Check Accreditation and Licensing: Ensure the facility is officially recognised and meets national healthcare standards.
- Evaluate Treatment Programs: Look for evidence-based medical detox, behavioural therapies, and holistic recovery approaches.
- Review Staff Qualifications: Confirm that doctors, therapists, and counsellors are trained and experienced in addiction treatment.
- Assess Aftercare Support: Ensure the centre provides follow-up programs, relapse prevention, and ongoing counselling.
- Consider Facility Amenities: Comfortable accommodations, nutrition, and wellness programs support recovery.
- Look for Personalised Care Plans: Treatment is tailored to the individual’s needs, substance type, and severity.
- Read Patient Reviews and Testimonials: Insights from former patients reveal the centre’s effectiveness and environment.
- Check Insurance and Cost Options: Verify coverage and affordability to ensure uninterrupted treatment.
What Are the Long-Term Preventive Strategies?
The long-term preventive strategies for de-addiction focus on sustaining recovery, reducing relapse risk, and promoting overall well-being. These strategies include ongoing therapy and counselling, maintaining a supportive social network, engaging in healthy lifestyle changes, avoiding high-risk situations, and participating in support groups or community programs.
Regular medical check-ups and mindfulness practices assist in monitoring progress and addressing stress, while education about substance abuse and coping skills equips individuals to handle triggers effectively. Meticulous routines, goal setting, and involvement in meaningful activities also fortify resilience, ensuring that recovery is maintained over the long term.
Is De-addiction Always Inpatient?
De-addiction is not always inpatient. Outpatient programs are effective for mild to moderate addiction, while severe cases require inpatient rehabilitation.
How Long Does De-Addiction Take?
The length of de-addiction varies; for instance, detox takes a week, but full rehabilitation and relapse prevention necessitate months to years.
Can De-Addiction Be Self-Managed?
No, de-addiction can hardly be self-managed. Self-efforts like quitting “cold turkey” rarely succeed long-term because of relapse risks. Organised programs are far more effective.
Does Insurance Cover De-Addiction Programs?
Yes. Insurance in a few countries covers many de-addiction programs, such as hospitalisation, medical detox, therapy, and sometimes aftercare. Coverage limits and pre-authorisation apply.